
The boy’s parents report no prior illnesses, and his immunizations are up-to-date. There was prolonged rupture of membranes and he was hospitalized for 3 days after delivery. His past medical history is notable for cesarean delivery at 36 weeks' gestation.
The boy’s parents state he did not vomit or have diarrhea. The infant drank 6 ounces about 4 hours before arrival, but would not feed at presentation. Given the girl’s lack of frank meningismus and improvement with ibuprofen, is a lumbar puncture indicated? What are the most common causes of meningitis in this age group? Should antibiotics be given?Ī 4-month-old boy presents with a history of cough, pallor, fever to 38.9☌ (102☏), and decreased feeding on the morning of presentation. Her peripheral white blood cell count is 16,000 with a left shift, and her chemistry is notable only for a glucose level of 146 mg/dL. An hour later, her vital signs are: temperature, 37.2☌ (99☏) heart rate, 126 beats/min respiratory rate, 20 breaths/min and blood pressure 111/67 mm Hg. The patient is given a 20 mL/kg normal saline bolus IV, 6 mg ondansetron IV, and 10 mg/kg ibuprofen orally. The remainder of her examination is normal.
#Viral vs bacterial meningitis csf findings full
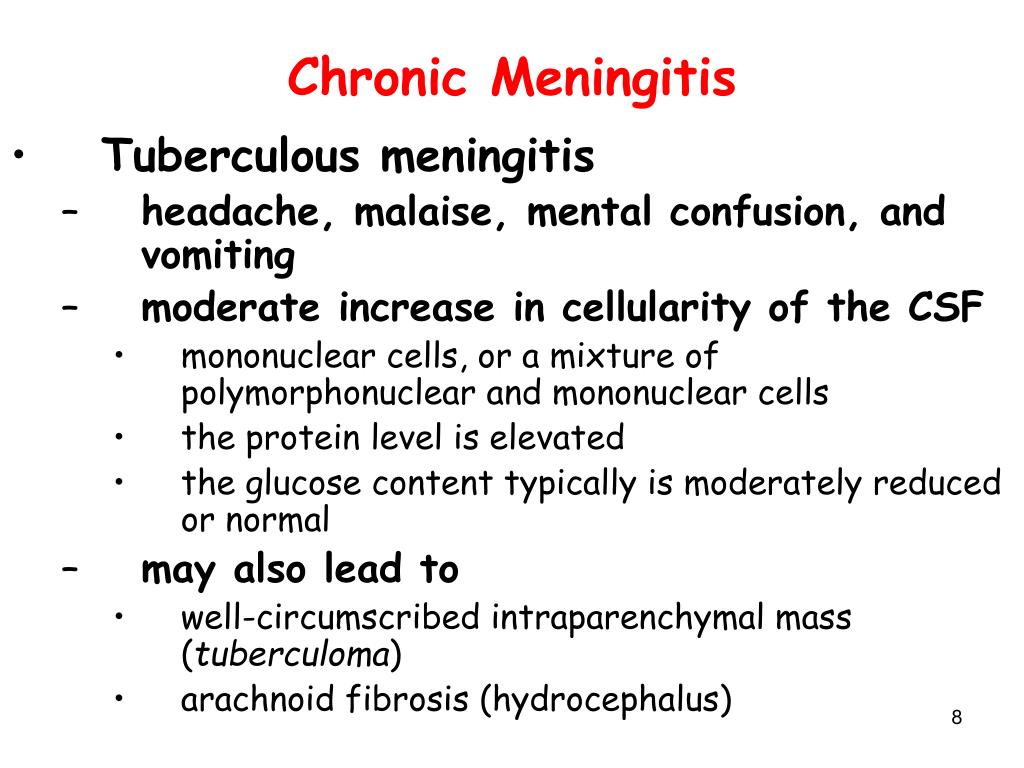
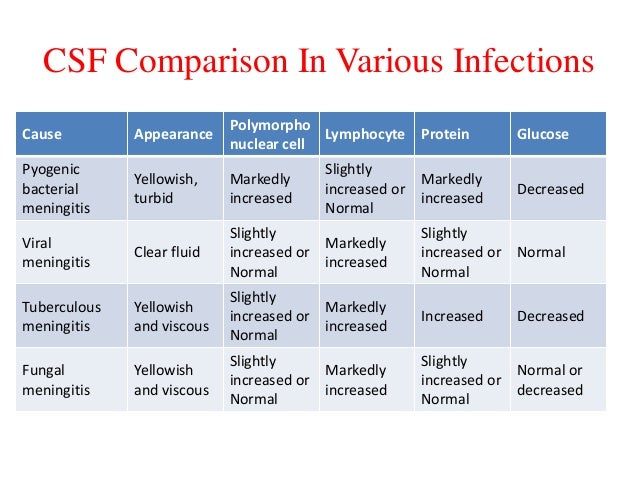
Her neck has full range of motion and she is negative for Kernig sign and Brudzinski sign. Her physical examination is notable for head and neck discomfort when moving from sitting to the supine position. Her vital signs are: temperature, 38.7☌ (101.6☏) heart rate, 142 beats/min respiratory rate, 22 breaths/min blood pressure, 119/77 mm Hg and oxygen saturation, 95% on room air. She had an episode of vomiting in triage. On physical examination, the child is tired but not toxic-appearing. The child took acetaminophen 2 hours prior to arrival. There has been no photophobia or rash, and there are no ill contacts. The patient arrives, ambulatory and alert, complaining of a bitemporal headache. The PA was concerned that she might have meningitis. Earlier that day, she was seen at her primary care physician’s office by a physician assistant who reported that the child had headache and fever intermittently for 3 to 4 days. On a warm day in June, an unvaccinated 9-year-old girl is sent to your ED. This issue provides evidence-based recommendations for the early identification and appropriate management of bacterial meningitis in pediatric patients. Although debated, corticosteroids should be considered in certain cases. Appropriate early antibiotic treatment and management for bacterial meningitis is critical for optimal outcomes. Inflammatory markers, such as procalcitonin, in the serum and cerebrospinal fluid may help distinguish between bacterial meningitis and viral meningitis. The presentation of bacterial meningitis can overlap with viral meningitis and other conditions, and emergency clinicians must remain vigilant to avoid delaying treatment for a child with bacterial meningitis. Pathogens That Cause Bacterial Meningitis, Based on Patient Age Risk Management Pitfalls in the Management of Pediatric Patients With Bacterial MeningitisĬlinical Pathway for the Management of Pediatric Patients With Suspected Bacterial Meningitis.Penetrating Trauma or Recent Neurosurgery The potential benefits of adjunct therapies, such as corticosteroids, and when they are indicatedĬausative Pathogens and Mechanisms of Infectionįindings That Indicate a Patient Should Undergo Lumbar PunctureĪntimicrobial Therapy for Patients Aged < 1 MonthĪntimicrobial Therapy for Patients Aged ≥ 1 Month Which antibiotic are recommended, and when they should be started How clinical prediction scores, such as the bacterial meningitis score, can help distinguish between bacterial meningitis and viral meningitis Inflammatory markers in the serum and cerebrospinal fluid, such as procalcitonin, can help detect serious bacterial illness Which physical examination findings indicate that a patient should undergo lumbar puncture Typical clinical findings that are consistent with bacterial meningitis and how they vary for patients in different age groups The most common causative pathogens, based on patient age If the presentation is not “classic” in nature, diagnostic and therapeutic delay can occur, frequently with devastating consequences. Since bacterial meningitis can present with many signs and symptoms, differentiation of bacterial meningitis from viral meningitis and from other mimics can be difficult.


 0 kommentar(er)
0 kommentar(er)
